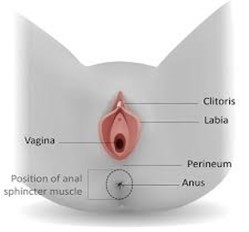
About the perineum
Your perineum is the area of tissue between your vagina and anus (back passage). It connects with your pelvic floor muscles and helps to support your pelvic organs.
About perineal trauma
During childbirth the perineum stretches to make room for your baby, and this makes the muscles and skin thinner.
As your baby is born the perineum can sometimes tear. Tears can occur in the perineum, labia (lips of the vagina) and inside the vagina.
Approximately 85% (85 out of 100) of women will sustain some degree of perineal trauma following the birth of their baby.
An episiotomy is a cut made by a doctor or midwife into the perineum to increase the vaginal opening and make more space for your baby’s birth.
We only perform an episiotomy with your consent and if it is clinically necessary.
Types of tear during childbirth
1st degree: small, skin-deep tear which usually heals naturally.
2nd degree: slightly deeper tear affecting both the skin and the muscles of the perineum. We recommend that we stitch (repair) all 2nd degree tears.
For some women the tear may be more extensive and need to be stitched in an operating theatre under an epidural or spinal anaesthetic. An obstetrician will perform this operation.
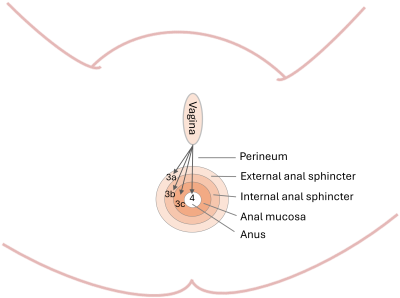
3rd degree: involves the skin, muscle and external anal sphincter (the muscle that surrounds the anus). These tears are classified according to their depth:
- 3a involves less than 50% of the external anal sphincter (EAS).
- 3b involves more than 50% of the EAS.
- 3c involves the whole of the EAS muscle and the internal anal sphincter muscle.
4th degree: extends further into the lining of the anus.
|
The type of tear you have is: __________________________________________________________________________ __________________________________________________________________________ |
About 3rd and 4th degree tears
A 3rd or 4th degree tear happens to about 3 in 100 women who have a vaginal birth. It is slightly more common in women having their first vaginal birth (6 out of 100 women). It happens to about 2 in 100 women who have a further vaginal birth.
Risk of 3rd and 4th degree tear
We cannot usually prevent a 3rd or 4th degree tear because we don't know it is going to happen. It is more likely to happen if:
- This is your first vaginal birth.
- Your baby weighs more than 4kgs (8lbs 8oz).
- Your baby is in a ‘back to back’ position (known as occipito-posterior or ‘OP’).
- You have a longer 2nd stage (‘pushing’ stage) of labour. This is because your tissues are stretched for longer.
- Your baby needs help to be born using ventouse (suction) or forceps.
- You have a quick labour and birth, where the perineal muscles do not have time to stretch and thin out.
- There is difficulty delivering your baby’s shoulders (known as shoulder dystocia).
- You have had a previous 3rd or 4th degree tear.
After surgical repair
When we have stitched your perineum, we will transfer you to the recovery area on the delivery suite.
You will have a drip in your arm to give you fluids until you are able to eat and drink.
You will also have a catheter (tube) in your bladder to collect your urine until you feel able to walk to the toilet. This usually takes 2 to 4 hours.
We use dissolvable stitches; they can take up to 3 months to dissolve completely.
Pain relief
We will offer you pain relieving drugs such as paracetamol, ibuprofen or diclofenac. When you get home, applying cool gel pads may help. If you use ice packs, wrap them in a clean cloth first. Do not put them directly onto your skin.
Antibiotics
We will recommend you take a course of oral (by mouth) antibiotics to reduce the risk of infection. This is because your stitches lie close to your anus.
Laxatives
We will recommend you take laxatives to make it easier and more comfortable to open your bowels.
It will be safe to breastfeed your baby while you are taking any of the medicines we offer you.
Looking after your perineum and stitches
Follow this guidance to look after your perineum and stitches.
Hygiene
- Wash your hands before and after you visit the toilet. This helps prevent the introduction of infection when you wipe yourself.
- Using a clean jug, pour warm water over your perineum when you pass urine (wee). The warm water will provide some comfort.
- After pooing, always wipe front to back, to avoid contamination from your back passage (anus).
- Change your sanitary pads frequently (about every 2 to 4 hours).
- Shower or bathe daily with plain water. Avoid putting soaps, shower gels or cosmetic products directly onto the area.
- Dry the area using a clean flannel or towel. Keep a separate flannel or towel for this area and change it every day.
- When you get home and have some privacy, you may find some relief by lying on an old towel without any clothing from the waist down. This means you can let your perineum ‘air dry’.
- Avoid wearing tight trousers or jeans.
Diet and fluids
- Drink plenty of water (about 2 to 3 litres a day). This will help dilute your urine (wee) and avoid irritation when you pass urine. It will also help you avoid dehydration (lack of fluids).
- Eating a healthy balanced diet will help you heal and avoid constipation. Try to include fibre, such as fresh fruit, vegetables, cereals, rice, pulses (lentils, chickpeas, beans) and wholemeal bread.
Opening your bowels (pooing)
- You can safely open your bowels without any damage to your perineum or stitches after the birth. The first few times you open your bowels, you can hold a clean pad against your perineum to protect your stitches and provide some support.
If there is a problem with your stitches
Your community midwife will offer to check your perineum at each visit. This will ensure your stitches are healing properly and there are no signs of infection.
Contact your community midwife or GP if:
- You develop swelling or throbbing pain in your perineum.
- Your stiches come apart and you observe the wound opening.
- You develop a high temperature or fever symptoms.
- You notice an unpleasant smell or abnormal discharge from the wound.
- You become incontinent (lacking control) for urine, faeces or wind.
If any of these symptoms develop, your midwife or GP will take a swab and may prescribe antibiotics for you.
Follow-up care
When you have been discharged by your community midwife, you will need to make an appointment to see your GP for your routine 6 to 8 week postnatal check.
We will also offer you the following appointments.
| Who you will see | When | Why |
|---|---|---|
| Telephone call with Perineal Specialist Midwife | 10 to 14 days | To discuss any concerns and make sure you have been given all necessary appointments |
| Perineal Specialist Midwife and Specialist Pelvic Health Physio (joint appointment) | 6 to 8 weeks | Assess wound healing and discuss postnatal recovery. Assess pelvic floor muscles and advise on pelvic floor exercises |
| Consultant Urogynaecologist | 4 to 6 months | Discuss your birth and any symptoms. Offer endoanal ultrasound scan. Advise on future birth planning. |
Re-starting sexual relations
In the weeks following a vaginal birth, many women feel discomfort because the vaginal canal can be dry, due to the readjustment of hormones.
There is no set time on when to re-start sexual relations. It depends on how you feel.
We advise you to wait until any bleeding has stopped and your perineal tear has healed.
It is normal to feel anxious about resuming a sexual relationship.
Sex may feel different at first and you may wish to experiment with sexual positions to find one that is comfortable for you. You may find it more comfortable to use a lubricant (to reduce friction).
Talk to your GP if sexual intercourse continues to be uncomfortable. They can give you the support you need.
Contraception
It is possible to conceive in the weeks following the birth of your baby, even before you have a period.
Talk to your GP or visit your local family planning clinic if you need contraception advice.
More information
NHS information on pelvic floor exercises and perineal health
NHS information on pelvic health classes
RCOG (Royal College of Obstetricians and Gynaecologists) information on 3rd and 4th degree tears
Contact information
Specialist Midwife for Perineal Health
Emails checked Tuesday, Wednesday and Thursday.
Email: krft.perinealhealth@nhs.net