About abdominal hysterectomy
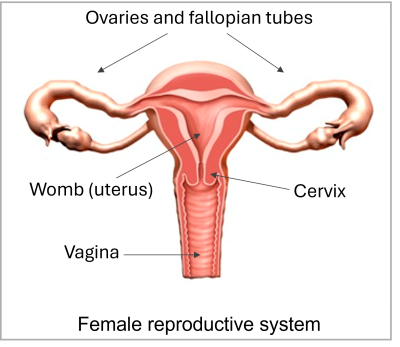
A hysterectomy is an operation to remove your uterus (womb). We usually remove your cervix (neck of your womb). It is also possible to remove your ovaries, but usually we leave them alone. We will discuss this with you before the operation.
If you decide against a hysterectomy or it is delayed
You may prefer to put up with your symptoms, rather than have the operation. Your gynaecologist will talk to you about the risks of not having the operation.
We will monitor your condition and try to control your symptoms.
Important
Contact your healthcare team if you experience any of the following:
- changes to your monthly bleeding pattern if you have periods
- increased abdominal (tummy) swelling
- worsening pain that needs more painkillers than you already take.
Benefits
We will discuss with you why we suggest you consider having a hysterectomy.
A hysterectomy may cure or remove the following conditions:
- Heavy or painful periods not controlled by other treatments.
- Fibroids, where part of the muscle of your womb becomes overgrown.
The following are less common reasons for having a hysterectomy:
- Endometriosis, where the lining of your uterus grows outside your uterus.
- Adenomyosis, where the lining of your uterus grows into the muscle of your uterus.
- Chronic pelvic inflammatory disease, where inflammation of your pelvis leads to chronic pain and often heavy periods.
- As part of treatment following abnormal cervical smear tests.
A hysterectomy may cure or improve your symptoms. However, pain may continue, depending on what causes it.
You will no longer have periods after a hysterectomy.
If we do not remove your ovaries, you may continue to have your usual premenstrual symptoms.
Alternative treatment
A hysterectomy is a major operation, usually recommended to women after simpler treatments have failed to control their symptoms.
For some women there may be no suitable alternatives and a hysterectomy may be recommended immediately, but this is unusual.
Your gynaecologist will discuss the following alternative treatments with you.
Heavy periods
- We can treat heavy periods using the following methods:
- A variety of non-hormonal and hormonal oral (by mouth) medicines.
- An IUS (intra-uterine system). This is an implant containing a synthetic form of the hormone progesterone that fits in your uterus.
- ‘Conservative surgery’ which removes only the lining of your womb (this is called endometrial resection).
- 'Conservative surgery' which prevents the lining of your womb from growing each month (this is called endometrial ablation).
Fibroids
Depending on the size and position of the fibroids, we can give you medicine to try to shrink them and control the symptoms.
We can also use surgery to remove the fibroids (myomectomy), or shrink the fibroids by reducing their blood supply (uterine artery embolisation).
Endometriosis and adenomyosis
We can treat heavy periods using the following methods:
- A variety of non-hormonal and hormonal oral (by mouth) medicines.
- An IUS (intra-uterine system). This is an implant containing a synthetic form of the hormone progesterone that fits in your uterus.
Chronic pelvic inflammatory disease
We can treat this with painkillers and antibiotics.
About the operation
We usually perform the operation while you are under a general anaesthetic (asleep). We can also use other anaesthetic techniques.
We may give you injections of local anaesthetic to help with pain, and antibiotics to help reduce the risk of infection.
During the operation [slightly edited]
During the operation we do the following.
- We may examine your vagina.
- We make a cut on your abdomen, usually on your 'bikini' line or downwards from your belly button (in some cases from above your belly button).
- We remove your womb and fallopian tubes, usually along with your cervix, through the cut. To remove your cervix we also need to make a cut at the top of your vagina.
- We may be able to remove only your womb (this is called a subtotal hysterectomy).
- We may need to remove your ovaries, even if this was not originally planned. We will discuss this with you before the operation.
- We may place a catheter in your bladder to help you to pass urine (wee).
- We may insert a drain (tube) in your abdomen to drain away fluid that can sometimes collect.
Risks and after-effects
Use the pull-down menus to see information on risks.
Common: more than 1 in 20
Discomfort: expected
It is normal to have some discomfort - which may include pain, irritation, or stiffness - for a few days or weeks after treatment. Pain relief options will be discussed with you.
Significant bleeding
Some bleeding is expected during most procedures, however significant bleeding may require further treatment. Usually it can be dealt with during the procedure, but may lead to a change from the planned procedure, need a blood transfusion, or need further emergency treatment.
Less common: fewer than 1 in 20
Conversion to subtotal hysterectomy
A conversion to a subtotal hysterectomy is where rather than a total hysterectomy (where the uterus and cervix is removed) being performed, the cervix is left behind due to technical difficulties.
If the cervix is not removed it is possible to have some ongoing menstrual bleeding, and as there is still a risk of cervical cancer developing in future the usual guidance remains in terms of cervical screening.
Significant bleeding
Some bleeding is expected during most procedures, however significant bleeding may require further treatment. Usually it can be dealt with during the procedure, but may lead to a change from the planned procedure, need a blood transfusion, or need further emergency treatment.
Rare: fewer than 1 in 100
Perioperative risks
There are a number of complications which having any operation increases the risk of - called perioperative risks ('peri' means 'around the time of'). These include allergic reactions and the risks of having an anaesthetic, which will be discussed with you by an anaesthetist.
Other complications include a chest, urinary, line, or other hospital-acquired infection, blood clots (deep vein thrombosis or pulmonary embolus), problems with the heart (including a heart attack), a stroke, memory problems or worsened kidney function. Any existing medical problem could also deteriorate.
Perioperative complications may increase the length of your hospital stay, require additional treatment including in some cases admission to intensive care, may be life threatening, and can lead to death.
Pre-operative assessment involves considering any investigations that may be appropriate prior to undergoing the operation. Undergoing these investigations, and any changes made based on these results, may reduce perioperative risks. Equally, it is not possible for pre-operative assessment to include testing for all possible conditions that may cause difficulties in the perioperative period.
There are a number of things that you can do in preparing for surgery to reduce the risks. This includes lifestyle changes such as exercising, maintaining a healthy diet, losing weight, and stopping smoking.
Compression injury
A compression injury describes any damage caused by pressure to tissues such as skin or nerves. This type of injury can occur in theatre as you are lying in one position for several hours. Any areas that are at risk, such as bony prominences, are padded during surgery to reduce the risk of compression injury. If this does occur you may experience numbness or a tingling sensation in the affected area, which is usually temporary.
Rarely, a complication called compartment syndrome can occur, where the pressure around the muscles in one of the limbs is too high, which may reduce the blood supply to those muscles. If this occurs, surgery may be required to release the pressure.
Damage to surrounding structures
Nearby structures are at risk of being injured during the procedure. For this operation there is a risk of injury to the bladder or ureters - the tubes which carry urine from the kidneys to the bladder (7 in every 1,000 patients), the bowel (4 in every 10,000 patients) and to major blood vessels.
In the very rare circumstance of significant injury this would usually be repaired immediately, but may need a larger cut in the middle of the tummy, and very rarely a stoma - an opening for faeces or urine on the front of your abdomen (tummy).
A bladder injury would usually be managed with having a catheter in place for 7-14 days after surgery.
In some cases, an oophorectomy or salpingectomy (removal of ovary or fallopian tube) is required, either due to injury or if unexpected disease is seen at time of operation.
There is a risk that damage is not noticed at the time of surgery, leading to symptoms in the days following surgery and potentially further surgery being required.
Common: more than 1 in 20
Wound complications
Wounds can sometimes be uncomfortable, become infected, heal more slowly than normal, may require special dressings to aid healing, or can reopen after they start to heal (dehiscence).
It is common to notice some mild redness, bruising, swelling, numbness, tingling or a burning sensation in and around the wound whilst it heals.
A wound infection is an infection of the skin or underlying tissues, where a cut has been made, often causing redness or swelling. It may require treatment with antibiotics. Occasionally, drainage of a collection of infected fluid (pus) or further surgery is also needed.
Delayed wound healing or wound dehiscence may require further treatment and in some cases surgery may be needed.
The risk of developing a wound complication is higher in some patients, including those who are obese, are smokers, and patients with diabetes.
Vaginal bleeding
Vaginal bleeding is when blood is passed from the vagina. Some bleeding should be expected for the first couple of weeks - similar to a light period, and may last for up to around 6 weeks. Pads should be used rather than tampons to reduce the risk of infection.
Pelvic infection (female)
A pelvic infection is an infection of the pelvis, and may include a urinary tract infection (UTI), or infection of the uterus, fallopian tubes, ovaries or other tissues in the pelvis. Infection in the pelvis can often be treated with antibiotics, but sometimes can lead to more serious infections – such as an abscess in the pelvis – and sepsis, and may require further treatment.
If you are concerned regarding significant pain, have a fever, or abnormal discharge you should seek medical advice.
Sluggish bowels (ileus)
An ileus, or temporary bowel paralysis, is when the bowel slows down following an operation or procedure. This can lead to pain in the abdomen, sickness and constipation.
It usually resolves in a few days but sometimes an X-ray or other investigations may be done to check the symptoms aren't being caused by something else.
Less common: fewer than 1 in 20
Incisional hernia
A hernia occurs when a part of the bowel pushes through the muscles in the tummy, often causing a lump. An incisional hernia is when the hernia is at the site of previous surgery. Bowel can get trapped in a hernia, and so further surgery may be needed to repair the hernia.
Urinary retention
Urinary retention is the medical term for having too much urine in the bladder and not being able to pass it. It is usually managed by temporarily placing a catheter into the bladder to allow the urine to drain out. This can happen due to bruising to some of the nerves in the pelvis and is the reason that the medical team may check that you are managing to empty your bladder appropriately after the operation. Should you have difficulty with emptying your bladder during the first week or so there are a number of different approaches possible. These can include passing a small urinary catheter just when needed, or going home with a catheter in the bladder for a week whilst things settle.
Premature ovarian insufficiency
Premature ovarian insufficiency, also known as premature/primary ovarian failure, is when the ovaries stop working normally, before the age of 40. There is around twice the risk of experiencing premature ovarian insufficiency compared to if the operation is not done. Symptoms - similar to those of natural menopause such as hot flushes, night sweats, irritability etc - may require hormone replacement therapy.
Ongoing symptoms
Despite the procedure, symptoms may continue. Depending on the context this may lead to further tests or treatments being recommended. This may include new or continuing urinary symptoms, pelvic pain and/or prolapse symptoms, depending on the indication for surgery. The likelihood of long-term ongoing symptoms is also heavily dependent on the original indication.
Rare: fewer than 1 in 100
Vaginal vault dehiscence
A vaginal vault dehiscence is where the line of sutures at the top of the vagina come apart. This usually requires emergency surgery to securely re-suture the top of the vagina.
Vesicovaginal fistula
A vesicovaginal fistula is an abnormal connection between the bladder and the vagina, leading to urine leaking from the vagina. Following a hysterectomy a fistula may also occur between the vagina and the ureter (the pipes that carry urine from the kidneys to the bladder).
A fistula most commonly develops around a week post-op and may require treatment to place a stent and/or catheter to allow the fistula to heal, these are left in place for around 4-6 weeks. Most heal over a few weeks, but surgical repair will sometimes be considered where the fistula is persisting long-term.
Rectovaginal fistula
A rectovaginal fistula is an abnormal passage or opening between the rectum and vagina. This may develop within weeks to months of the original surgery and usually requires surgical repair.
Need to go back into theatre
Due to complications following the operation it may be advised to have a further operation during the hospital stay. After this operation this would usually be due to ongoing bleeding, to drain a collection of blood at the top of the vagina, or because of wound complications.
Blood clots (deep vein thrombosis or pulmonary embolus) – 1 in 300 chance
Blood clots can form in the veins of the legs (deep vein thrombosis), causing pain and redness in the leg, and are more likely to occur after a procedure or operation, when people tend to move around less.
These clots can occasionally also travel from the legs to the lung (pulmonary embolus), and can cause problems with breathing. Clots in the leg or lung require treatment such as with blood thinning medications. More rarely a large pulmonary embolism can be life threatening.
Getting moving early after treatment reduces your risk of clots. You may also be advised to wear compression stockings or calf compression pumps and have blood thinning injections following treatment to help reduce the risk of clots. This depends on the treatment you are having and your medical history.
Vaginal vault haematoma (collection of blood) - 1 in 500 chance
A haematoma is a collection of blood within the body, outside of a blood vessel. This can occur at the top of the vaginal canal (vaginal vault). It can sometimes be left to be reabsorbed by the body with time, but will often need a procedure or operation to drain the blood.
Pelvic abscess - 1 in 500 chance
A pelvic abscess refers to a pocket of infected fluid - pus - in the pelvis. Antibiotics are usually needed, but abscesses are difficult to treat with antibiotics alone so a procedure or operation to drain it may be needed.
Death – 1 in 3,000 chance
There is a risk of dying either directly due to the procedure or treatment, or from complications in the subsequent days or weeks. The risk is dependent on many factors including your age and any underlying medical problems you may have. Any likelihood presented will usually reflect the risk of death within 30 days of the proposed treatment. Overall the risk of death within six weeks of the operation is approximately 1 patient in every 3,000.
Common: more than 1 in 20
Symptomatic abdominal adhesions
Abdominal adhesions are bands of scar tissue that can develop between structures in the abdomen and pelvis - for example between loops of bowel - after surgery.
Occasionally, these bands can cause symptoms and complications, for example causing abdominal or pelvic pain, or causing the bowel to become blocked. Where a bowel obstruction occurs this may require surgery or other treatment to resolve the blockage.
Dyspareunia (discomfort during sex)
Dyspareunia is the medical term for experiencing pain during sexual intercourse (sex). Sexual intercourse should be avoided during the first six weeks as the area heals. Some discomfort should be expected during the following weeks.
Less common: fewer than 1 in 20
Abnormal scarring
If the skin is injured, whether by surgery or other means, a scar is formed during the healing process. Normally scars will fade and become paler over time, but do not completely disappear.
Abnormal scarring is when a wound heals leaving a scar that is either larger or a different colour (hypertrophic or keloid scar), or more uncomfortable than is typical. This can occur more often if a wound has taken a long time to heal, and in certain skin types.
Vaginal vault prolapse
A vaginal vault prolapse is where the top of the vagina (vaginal vault) drops down into the vaginal canal.
After-effects of the operation
You can expect the following after-effects.
- Pain. We will give you medicine to control this. Take it as instructed so that you can move about and cough freely.
- Scarring of your skin.
- Sometimes the wound opens after the operation. In this situation, we give you another procedure to fix it.
- You will no longer have periods.
- You will not be able to get pregnant.
Recovery and returning to everyday activities
After the operation we will transfer you to the recovery area and then to the ward. We may give you fluid for 12 to 24 hours through a drip (small tube) in a vein in your arm.
You will probably feel some pain or discomfort when you wake and we may give you strong painkillers. Pain relief is an important part of your recovery. Tell your healthcare team if you are in pain.
If you have a catheter or drain, we usually remove them after 4 to 6 hours.
We usually remove the drip after 12 to 24 hours.
We will allow you to start drinking and eating light meals.
You may get a slight discharge or bleeding from your vagina for the first 2 weeks. Tell your healthcare team if this becomes heavy. Use sanitary pads, not tampons.
You may get wind pains on day 2 or 3. We can give you medicine to relieve this.
You will be able to go home when your gynaecologist decides you are medically ready, which is usually after 3 to 5 days.
Nutrition and exercise
We advise you to drink plenty of fluid and increase the amount of fibre in your diet to avoid constipation.
We may recommend exercises to help you recover. Getting out of bed and walking is an important part of your recovery. We may also give you breathing, pelvic floor or other exercises to do. Try to do these, even if you do not feel like it.
Returning to everyday activities
- To reduce the risk of a blood clot, follow our instructions if we give you medicine or ask you to wear special stockings.
- Rest for 2 weeks and continue to do the gentle exercises we give you. Try to take a short walk every day.
- Regular exercise will help you to return to normal activities as soon as possible. Before you start exercising, ask your healthcare team or GP for advice.
- Eat healthily, drink plenty of fluid and rest when you need to.
You can return to work once your doctor has said you are well enough to do so. For most people this is after 6 to 8 weeks, depending on the type of work they do.
Most people feel more or less back to normal after 3 months.
While you recover, do not:
- Do not drive or ride a bike until you are confident about controlling your vehicle, including in an emergency. Check your insurance policy first and speak to your doctor if you have concerns.
- Do not have sex for at least 6 weeks and before any bleeding or discharge has stopped. When you have sex again, it can be uncomfortable at first and you may need to use a lubricant.
- Do not stand for too long or lift anything heavy.
In hospital and after discharge home
Tell your healthcare team if you experience any of the following:
- heavy bleeding
- increasing pain
- shortness of breath.
Menopause and HRT
If your hysterectomy is performed while you are still having periods and your ovaries are removed during the operation, it is likely you will have menopausal symptoms.
These may include hot flushes, night sweats, passing urine more often, a dry vagina, dry skin and hair, mood swings and lack of sex drive. You can usually treat these symptoms with HRT.
Your GP is likely to recommend you take HRT until the time when you would have gone through menopause naturally (at about age 50 to 52). You can carry it on for longer if you want to. Discuss this with your GP.
Most women take HRT in tablet form but it is also available as patches, gels, nasal sprays, vaginal rings and implants. Your GP can discuss these options with you.
If we do not remove your ovaries
Your ovaries should continue to produce the hormones you need until you have reached the normal age of menopause. However, there is some evidence to suggest that some women who have had a hysterectomy may start menopause 2 to 3 years earlier.
After a hysterectomy, it can be more difficult to know when you are in menopause, as your periods will have stopped. You may need blood tests.
If you develop flushes or sweats or other menopausal symptoms, talk to your GP about HRT.
Contact information
Kingston Hospital Gynaecology Department
Telephone:
Gynaecology Administrative Service: 020 8934 6407
Gynaecological Clinical Nurse: 020 8934 6326
Email: khn-tr.gynaecology@nhs.net