About vaginal hysterectomy
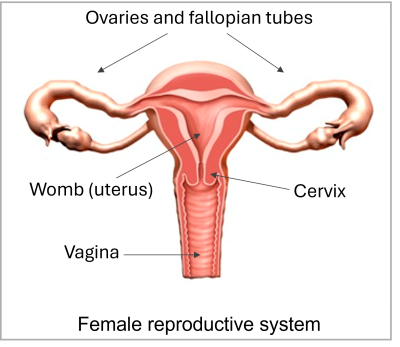
A vaginal hysterectomy is an operation to remove your uterus (womb) and cervix (neck of your womb) through your vagina.
It is also possible to remove your ovaries, but usually we leave them alone. We will discuss this with you before the operation.
If you decide against a hysterectomy or it is delayed
You may prefer to put up with your symptoms, rather than have a hysterectomy. Your gynaecologist will talk to you about the risks of not having the operation.
We will monitor your condition and try to control your symptoms.
Important
Contact your healthcare team if you experience any of the following:
- changes to your monthly bleeding pattern if you have periods
- increased abdominal (tummy) swelling
- worsening pain that needs more painkillers than you already take.
Benefits
We will discuss with you why we suggest you consider having a hysterectomy.
A hysterectomy may cure or remove the following conditions:
- Heavy or painful periods not controlled by other treatments.
- Fibroids, where part of the muscle of your womb becomes overgrown.
- Uterine prolapse, where your womb drops down. This is caused by the support tissues of your womb becoming weak.
The following are less common reasons for having a hysterectomy:
- Endometriosis, where the lining of your uterus grows outside your uterus.
- Adenomyosis, where the lining of your uterus grows into the muscle of your uterus.
- Chronic pelvic inflammatory disease, where inflammation of your pelvis leads to chronic pain and often heavy periods.
- As part of treatment following abnormal cervical smear tests.
A hysterectomy may cure or improve your symptoms. However, pain may continue, depending on what causes it.
You will no longer have periods after a hysterectomy.
If we do not remove your ovaries, you may continue to have your usual premenstrual symptoms.
Alternative treatment
A hysterectomy is a major operation we usually recommend to women after simpler treatments have failed to control their symptoms.
For some women there may be no suitable alternative and we may recommend a hysterectomy immediately, but this is unusual.
There are alternative methods to treat some common conditions.
Uterine prolapse
Doing pelvic floor exercises may improve your symptoms. Depending on your age, a pessary (a ring that fits into your vagina) may prevent your womb from dropping down.
Heavy periods
- We can treat heavy periods using the following methods:
- A variety of non-hormonal and hormonal oral (by mouth) medicines.
- An IUS (intra-uterine system). This is an implant containing a synthetic form of the hormone progesterone that fits in your womb.
- ‘Conservative surgery’ which removes the lining of your womb or prevents it from growing each month.
Fibroids
Depending on the size and position of the fibroids, we can give you medicine to try to shrink them and control the symptoms.
We can also use surgery to remove the fibroids, or shrink the fibroids by reducing their blood supply.
About the operation
We usually perform the operation while you are under a general anaesthetic (asleep). We can also use other anaesthetic techniques.
We may give you antibiotics during the operation to reduce the risk of infection.
- We make a cut around your cervix at the top of your vagina. We separate your womb and remove it. We may remove your ovaries, although this is not always possible.
- We usually stitch your womb to reduce the risk of a future prolapse.
- We may place a pack (like a large tampon) in your vagina.
- We may place a tube (catheter) in your bladder to help you pass urine (wee).
The operation usually takes about 45 minutes.
In hospital and after discharge home
Tell your healthcare team if you experience any of the following:
- heavy bleeding
- increasing pain
- shortness of breath.
Complications and risks
xxx
After-effects of the operation
You can expect the following after-effects.
- Pain. We will give you medicine to control this. Take it as instructed so that you can move about and cough freely.
- You will no longer have periods.
- You will not be able to get pregnant.
Recovery afterwards
After the operation we will transfer you to the recovery area and then to the ward. We may give you fluid through a drip (small tube) in a vein in your arm.
You will probably feel some pain or discomfort when you wake and we may give you strong painkillers. Pain relief is an important part of your recovery. Tell your healthcare team if you are in pain.
We usually remove the drip, the pack in your vagina and the catheter some time over the next day or two.
We will allow you to start drinking and eating light meals. Good nutrition will speed up your recovery.
On the second or third day, you may get wind pains. These can last for 1 to 2 days, but we can offer you medicine to relieve them.
You will be able to go home when your gynaecologist decides you are medically ready, which is usually the same day or after 1 to 3 days.
You may get a slight discharge or bleeding from your vagina for the first 2 weeks. Tell your healthcare team if this becomes heavy. Use sanitary pads, not tampons.
Nutrition and exercise
We advise you to drink plenty of fluid and increase the amount of fibre in your diet to avoid constipation.
Your healthcare team may recommend exercises to help you to recover. It is important to get out of bed and walk. We may give you breathing or other exercises. Do these, even if you feel you do not want to. They will speed up your recovery.
Recovery afterwards
After the operation we will transfer you to the recovery area and then to the ward. We may give you fluid through a drip (small tube) in a vein in your arm.
You will probably feel some pain or discomfort when you wake and we may give you strong painkillers. Pain relief is an important part of your recovery. Tell your healthcare team if you are in pain.
We usually remove the drip and the pack in your vagina and the catheter some time over the next day or two.
We will allow you to start drinking and eating light meals. Good nutrition will speed up your recovery.
On the second or third day, you may get wind pains. These can last for 1 to 2 days, but we can offer you medicine to relieve them.
You will be able to go home when your gynaecologist decides you are medically ready, which is usually the same day or after 1 to 3 days.
You may get a slight discharge or bleeding from your vagina for the first 2 weeks. Tell your healthcare team if this becomes heavy. Use sanitary pads, not tampons.
Nutrition and exercise
We advise you to drink plenty of fluid and increase the amount of fibre in your diet to avoid constipation.
Your healthcare team may recommend exercises to help you to recover. It is important to get out of bed and walk. We may give you breathing or other exercises. Do these, even if you feel you do not want to. They will speed up your recovery.
Returning to everyday activities
To reduce the risk of a blood clot, follow our instructions if we give you medicine or ask you to wear special stockings.
Rest for 2 weeks and continue to do the gentle exercises we give you. Try to take a short walk every day.
Regular exercise will help you to return to normal activities as soon as possible. Before you start exercising, ask your healthcare team or GP for advice.
Eat healthily, drink plenty of fluid and rest when you need to.
You can return to work once your doctor has said you are well enough to do so. For most people this is after 4 to 6 weeks, depending on the type of work they do.
Most people feel more or less back to normal after 2 to 3 months.
While you recover, do not:
- Do not drive or ride a bike until you are confident about controlling your vehicle, including in an emergency. Check your insurance policy first and speak to your doctor if you have concerns.
- Do not have sex, use tampons or get into the bath, swimming pool or hot tub for at least 12 weeks and before any bleeding or discharge has stopped. When you have sex again, it can be uncomfortable at first and you may need to use a lubricant.
- Do not stand for too long or lift anything heavy.
Menopause and HRT
If your hysterectomy is performed while you are still having periods and your ovaries are removed during the operation, it is likely you will have menopausal symptoms.
These may include hot flushes, night sweats, passing urine more often, a dry vagina, dry skin and hair, mood swings and lack of sex drive. You can usually treat these symptoms with HRT.
Your GP is likely to recommend you take HRT until the time when you would have gone through menopause naturally (at about age 50 to 52). You can carry it on for longer if you want to. Discuss this with your GP.
Most women take HRT in tablet form but it is also available as patches, gels, nasal sprays, vaginal rings and implants. Your GP can discuss these options with you.
If we do not remove your ovaries
Your ovaries should continue to produce the hormones you need until you have reached the normal age of menopause. However, there is some evidence to suggest that some women who have had a hysterectomy may start menopause 2 to 3 years earlier.
After a hysterectomy, it can be more difficult to know when you are in menopause, as your periods will have stopped. You may need blood tests.
If you develop flushes or sweats or other menopausal symptoms, talk to your GP about HRT.
Contact information
Kingston Hospital Gynaecology Department
Telephone:
Gynaecology Administrative Service: 020 8934 6407
Gynaecological Clinical Nurse: 020 8934 6326
Email: khn-tr.gynaecology@nhs.net